The Opioid Crisis: How You Can Help
 Reviewed by Lisa Alizadeh, Licensed Professional Counselor
Reviewed by Lisa Alizadeh, Licensed Professional Counselor
The U.S. Department of Health and Human Services declared the opioid crisis a public health emergency in 2017. This designation led to the release of a five-point strategy to fight the epidemic, which includes: improving access to treatment, prevention, and recovery services; increasing access to overdose-reversing drugs; strengthening data collection and reporting; helping to advance research on pain management and addiction; and improving pain-management practices.
While the crisis continues, this increased attention by policymakers shows there is potential to make a change. And with it are many ways to join the fight to end the opioid epidemic, which you’ll learn more about here.
The Growth of the Opioid Crisis
What are Opioids?
Prescription opioids are commonly used for anesthesia and pain management. Common prescription opioids include oxymorphone, codeine, fentanyl, hydrocodone, and morphine. They’re generally considered safe if used for short periods of time and in controlled settings by low-risk patients. However, because opioids are highly addictive, and the misuse of prescribed drugs can also lead to heroin use, physicians are taking greater care in prescribing opioids.
Opioid prescription rates have declined steadily in recent years. The Centers for Disease Control and Prevention (CDC) notes that prescription rates dropped from 72.4 prescriptions per 100 persons in 2006 to 58.5 in 2017, which is showing progress. However, much more attention is being placed on prescribing practices as overdose deaths from opioids remain strikingly high.
-Anne Schuchat, M.D., Principal Deputy Director, Centers for Disease Control and Prevention
In 2016, in response to the opioid epidemic, the Centers for Disease Control and Prevention (CDC) released updated guidelines on opioid prescribing practices, including suggestions for assessing patient risk factors. While not everyone who is prescribed opioids is likely to become addicted, many factors may indicate that the person is at higher risk for addiction. Some of those, according to the Mayo Clinic, include poverty, unemployment, family and personal history of substance use disorders, depression and anxiety, and/or heavy tobacco use. With those risk factors in mind, regulatory agencies, healthcare providers, and medical schools are becoming increasingly vigilant about prescribing practices and working to limit the rise in opioid deaths.
The Opioid Epidemic
Over recent years, deaths from opioid overdoses have risen steadily and rapidly, increasing from a little more than 3,000 in 2010 to 47,600 in 2017. The CDC says the first wave of the epidemic began in the early 1990s when opioid prescription rates increased drastically. The second wave began in 2010 when the rates of heroin overdoses increased. We’re currently experiencing the third wave of the epidemic, which started in 2013 and is linked fentanyl, a synthetic opioid most commonly used as anesthesia.
A 2019 article in Nature provides compelling insights about the rise of opioid use in the U.S. It explains that the epidemic resulted from a perfect storm of circumstances, including changes in pain-management treatment, the surge in marketing of opioid medications (in particular OxyContin, manufactured by Purdue Pharma, which has received increased scrutiny and even litigation over its role in the opioid crisis); vulnerability of the U.S. healthcare system, making physicians more prone to defer to pharmaceutical companies’ advice in pain management; and the convergence of other crises, such as economic declines.
Where the Epidemic Has Hit Hardest
From any map of overdose rates, the northeastern U.S. seems to be hit the hardest by the opioid crisis. The National Institute on Drug Abuse (NIDA) reports that the following states experienced the highest rates of opioid deaths in 2017:
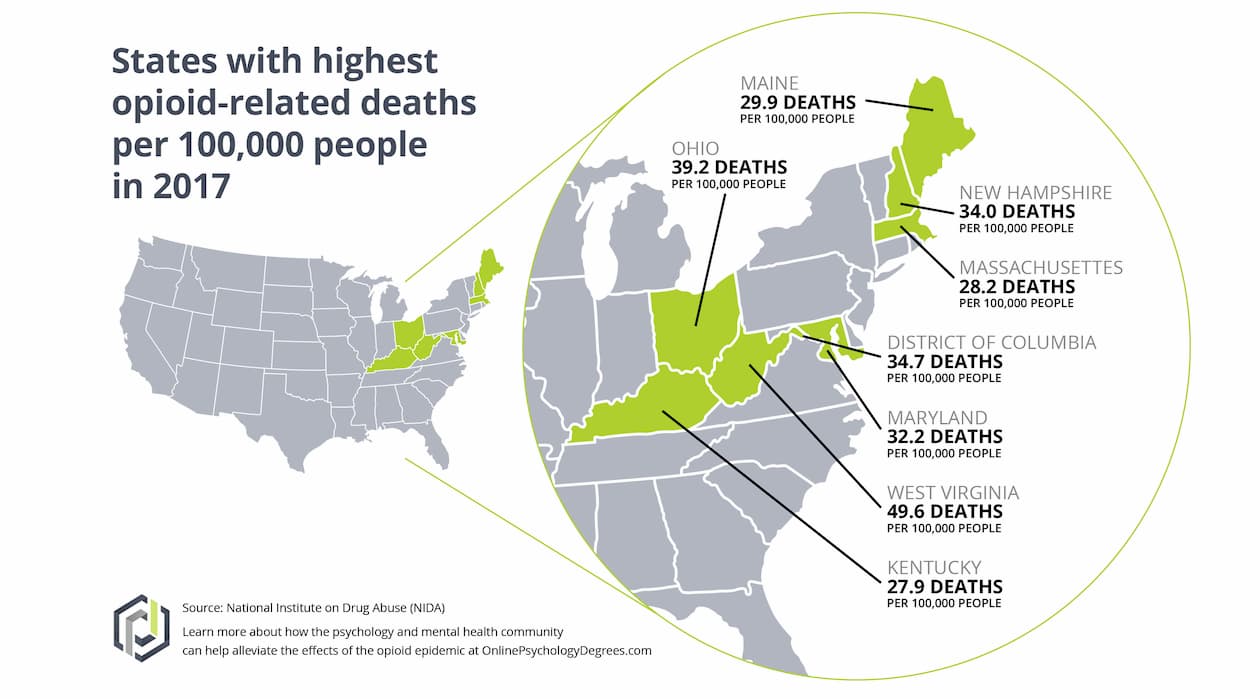
| State | Opioid-Involved Deaths in 2017 |
| West Virginia | 833 |
| Ohio | 4,293 |
| District of Columbia | 244 |
| New Hampshire | 424 |
| Maryland | 1,985 |
| Maine | 278 |
| Massachusetts | 1,913 |
| Kentucky | 1,160 |
The information in this table is ranked in order of opioid-related death rates. Overall population size determines these statistics.
While many of these states are in the eastern United States, the CDC emphasizes that no state or community is immune to the opioid crisis. Both metropolitan and non-metropolitan areas are affected, albeit in different ways. Research from 2017 indicates that heroin and synthetic opioid deaths were higher in metropolitan areas, while fatalities from natural or semisynthetic opioids were higher in non-metropolitan regions.
The opioid crisis isn’t only affecting the U.S. A 2017 United Nations report found that two-thirds of drug deaths globally were opioid-related. Canada, the United Kingdom, and other parts of Europe are experiencing higher rates of opioid overdose deaths.
Who is Affected?
Just as the epidemic touches all regions, it affects all demographic groups. However, a study published by National Vital Statistics Reports about opioid deaths reveals that men are three times more likely to die from an overdose. A 2019 Kaiser Health News report posits that one reason men die more frequently of overdose is that they’re more likely to use drugs without others nearby, making it less likely that their overdoses will be seen, reported, or treated.
The CDC study also shares grim new information: While almost every age group saw a rise in opioid-related death rates, the most significant increase was among young people ages 25 to 34.
Socioeconomic factors are most certainly a part of the crisis as well. The National Institute on Minority Health and Health Disparities noted that between 2012 and 2015, the counties with high unemployment, lower education levels, and low median incomes experienced the highest overdose death rates, and these factors seemed to affect white Americans disproportionately.
The heartbreaking truth is that almost all communities in the U.S. are affected by this epidemic. Not only does it affect the people with addiction, but it also affects their friends and families, who witness the decline of their loved ones with little hope and all too often must grieve their deaths.
But there is hope. Because of the increased attention directed toward the opioid crisis, more resources are becoming available. The battle is being fought on many different fronts, with experts and professionals from many fields working to bring about change, including those in mental health, public health, public policy, social services, and advocacy. Numerous ways to get involved and to help reverse this epidemic are being developed and implemented.
The Effects of the Opioid Crisis on Mental Health Professionals
Mental health professionals are essential in helping combat the opioid crisis. They are on the frontlines of providing substance-use disorder treatment, supporting patients with depression and anxiety (issues often related to addiction), and counseling families and loved ones of people with addictions. While essential in the fight against the opioid crisis, the work is challenging and can take a toll on providers’ own mental health.
A decades-long shortage of clinicians who treat substance use disorders has only worsened since the rise of the opioid crisis. Low staffing also requires providers to take on even more work. Overall, being overworked and emotionally strained can cause burnout. This has not gone unnoticed, however.
In 2018, the Health Resources & Services Administration (HRSA) released a set of behavioral health workforce projections for 2016 through 2030, which acknowledges those gaps that are intensified by high turnover, low pay, and a lack of trained professionals. With these statistics in hand, the National Council for Behavioral Health is working with the federal government to find ways to close those gaps. One such approach is loan-forgiveness programs for those entering the profession to combat addiction—part of a comprehensive opioid package signed into law in 2018. Hopefully, this promising investment will lead to an increase in the number of professionals who can help combat addiction.
Identifying Opioid Addiction: Symptoms and Signs
The American Psychological Association (APA) defines addiction as a “chronic disorder with biological, psychological, social, and environmental factors influencing its development and maintenance.” Its website also notes that around half of the risk for addiction is genetic. What’s essential here is that addiction isn’t any one person’s fault—not the person with the addiction nor that person’s family or friends. It is, sadly, a part of the human experience. But it is treatable, and those with addiction can be helped.
While it might be hard at first to see symptoms that someone you know is addicted to opioids, the following signs could be a potential indicator a friend or loved one is addicted to opioids (according to the National Institute on Drug Abuse and the American Society of Anesthesiologists). Note that many of these signs also may be associated with depression or anxiety, which are often linked to opioid use:
Supporting a Loved One With Opioid Addiction (Even If You Are Not a Therapist)
Preparing to Help
The first thing to do is to acknowledge there is an addiction and then to educate yourself about it. The American Addiction Center emphasizes that addiction is not a moral failing; it is a disease. Understanding this is an essential part of genuinely offering support to your loved one. Learn more about addiction and even seek out therapy yourself to identify ways to best support your friend or family member who is struggling with addiction.
To educate yourself, look into the following:
How to Approach Someone About Their Addiction
The next step after educating yourself is to approach your loved one. Because addiction and its corresponding symptoms can cause rifts in your relationship, it’s essential to approach your loved one with compassion and love. This person is struggling, and it’s the disease that is causing the rifts, not the person.
One of the first considerations is timing. You don’t want to approach someone who is under the influence when you’re ready to have this meaningful discussion. Make sure that the person is clearheaded and in an environment that feels loving and safe.
It can be challenging knowing how to discuss your concerns. The Hazelden Betty Ford Clinic says there’s no perfect way. If it feels appropriate, it can be helpful to bring someone who has also has experienced addiction or to have that person available by phone. Having someone who has gone through recovery be part of this discussion can help establish trust and show that recovery is possible.
StartYourRecovery.org provides some helpful ways to start the conversation suggestions for what questions you can ask. Questions such as, “I wanted to check in with you because you haven’t seemed yourself lately,” and, “I’ve been worried about you lately,” demonstrate your concern, compassion, and love for the person. Then you can delve more deeply by asking:
The Hazelden Betty Ford Clinic also has recommendations about what to say to a variety of people in your life, including co-workers, partners, or friends.
From there, you can assist them in seeking resources to get the help they need. This is where your prior research about treatment options will come in helpful. Having thought about it, you can present your ideas and thoughts and get feedback. Again, it might be useful to have someone who has experienced addiction to help guide the process.
Do’s and Don’ts for Bringing Up a Loved One’s Addiction
Here are some do’s and don’ts for how to go about this (sources: VeryWell Mind, American Addiction Center):
| Do | Don’t |
| Show love and build trust by expressing compassion. | Be negative or accusatory. This can trigger shame and guilt, which hinders recovery. |
| Speak and show optimism and provide encouragement. | Threaten, punish, or criticize the person if recovery comes slowly (it likely will). |
| Be honest and open about your feelings. Use “I” statements. | Skirt around your feelings or blame the person with addiction for your own emotions. |
| Set and be consistent with your expectations, promises, and consequences. | Make any promises you cannot keep. |
| Help them address underlying reasons for the addiction. Show them that they are not alone and that resources and people are there to support and help them through the process. | Place all of the responsibility on the person with an addiction. |
| Respect their privacy. | Force them to share everything they have experienced or give you a play-by-play of daily activities. |
| Understand that recovery is a lifelong process. | Expect them to change immediately. Recovery is a long process, and it might take several failed sobriety attempts. |
Supporting a Loved One During Treatment
The do’s and don’ts referenced above continue when supporting someone during treatment. What’s important to understand, though, is that there is no magical treatment that will make the addiction go away immediately.
Treatment for addiction can be a long and painful process. It’s going to take resiliency and compassion to help them through this process. This Psychology Today article provides a dozen recommendations for supporting someone with an addiction—two of which are especially necessary as the person is in recovery: Don’t give up, and take care of yourself. Below you’ll find some tips on self-care.
Providing Support After Treatment Is “Completed”
While it’s important to celebrate a person’s treatment, overcoming addiction is a lifelong process and requires constant support. The Substance Abuse and Mental Health Services Administration (SAMHSA) outlines the four primary elements to support recovery:
- Health: You can assist your loved one in managing their disease by helping them stay healthy in general. Part of this is helping to keep them sober, but supporting them to make healthy lifestyle choices through healthy eating and physical activity also is helpful.
- Home: As someone close to this person, you can ensure they have a stable and safe place to live to help maintain sobriety.
- Purpose: You can help them find meaning in life, which includes day-to-day independence by earning a regular income, and helping them participate in society by finding meaningful activities.
- Community: Social networks and relationships are what help a person maintain their recovery. You can provide them with love, friendship, and hope, and you can encourage other loved ones to show their support.
Beyond these four elements, continuous therapy for both the person with the addiction and yourself is crucial. Additionally, if your spouse, partner, child, or parent is experiencing addiction, family therapy can be extremely valuable in navigating recovery as a family.
What Can Psychologists Do for Those with Opioid Addictions?
Because one of the most significant risk factors of opioid misuse is experience with mental health issues such as depression and anxiety, psychologists can play an essential role in helping patients with opioid addictions.
Preventing Opioid Addiction
A June 2019 APA article by Zara Greenbaum highlights recent research that shows how psychologists can prevent, diagnose, and treat opioid addiction most effectively:
Treatment for Addicted Patients
Because not everyone can be prevented from experiencing opioid addiction, psychologists also play an essential role in treatment. A 2017 American Psychological Association article highlights some treatment methods for psychologists.
In addition, as addiction is often co-morbid with other mental health diagnoses, dual diagnosis treatment is frequently recommended. This method is used to help those who have both an addiction and a separate mental health diagnosis or behavioral disorder. Co-occurring disorders require different treatment, as the brain responds differently with additional diagnoses, genetics play a significant role, and there are triggers beyond those solely for addiction; for instance, a traumatic event may affect a person with dual diagnoses in a manner unlike it would for those who solely have an addiction diagnosis.
Careers Working with People with Addictions
Also called “addiction counselors,” substance abuse counselors provide therapy and intervention for people facing addiction to help them through the recovery process. Typically, these providers would be certified as a Substance Abuse Counselor (CSAC or SAC) or Alcohol and Other Drug Abuses (AODA) Counselor.
Mental health counselors work with patients facing a broader set of mental health challenges, including anxiety, depression, and grief that can be linked to, or make them more at risk for, addiction. Mental health counselors often hold the title of Licensed Professional Counselor (LPC).
Psychologists study human behavior and can work with patients in both therapeutic and research settings. Those explicitly focused on substance use disorders can participate in studying the psychological impacts and causes of opioid addiction as well as work with patients directly through counseling. These psychologists will either have a Ph.D. or PsyD in clinical or counseling psychology and specialize within the area of substance use disorders.
Because addiction to substances can have an impact on relationships, marriage, and family therapists are there to counsel patients and their families through the recovery and addiction-management process. These providers will hold the title of Licensed Marriage and Family Therapist (LMFT).
Social workers are often at the frontlines of the opioid crisis by working directly with vulnerable populations who might be more at risk of addiction and diagnosing and referring clients to resources further treatment. These providers can work in case management roles with a Master’s in Social Work (MSW) or as counselors with the certification Licensed Clinical Social Worker (LCSW).
How to Take Care of Yourself When Helping a Person with Addiction
“Compassion fatigue” or “burnout” are terms commonly used when describing how people in the helping professions (e.g., counselors, medical professionals, and clergy) are affected by working with people with diseases, who are in distress, or who are particularly vulnerable. These terms can be applied to loved ones as well. The absorption of clients’ and family members’ pain is particularly relevant for mental health workers working to treat those with substance use disorders and their loved ones. Burnout can lead to adverse physical and mental health outcomes for caregivers, but signs can also be challenging to identify.
If you work in any capacity with someone or have a loved one who is addicted to opioids or other drugs, prioritizing your self-care is essential for you to have the energy and ability to continue your work and support. Here are some tips on what you can do to take care of yourself:






